Mpox is a rare disease that can make you sick, including a characteristic rash. People often, but not always, have an earlier flu-like illness.
If you develop a new rash that looks like Mpox, talk to your health care provider, even if you don’t think you had close contact with someone with Mpox.

Images courtesy of UK Health Security Agency
Mpox Vaccine
Mpox vaccine is available to people who are eligible at a number of Health District and community clinics.
Weekly Mpox Data
Probable and Confirmed Cases
in Clark County as of December 22, 2025
333
Estimated Vaccines Administered
in Clark County by SNHD-affiliated clinics as of December 22, 2025
12,413
NOTE: Case count and vaccines administered data are cumulative and includes data beginning in June 2022. For weekly case reports go to www.southernnevadahealthdistrict.org/Health-Topics/monkeypox/reports/.
Mpox FAQ
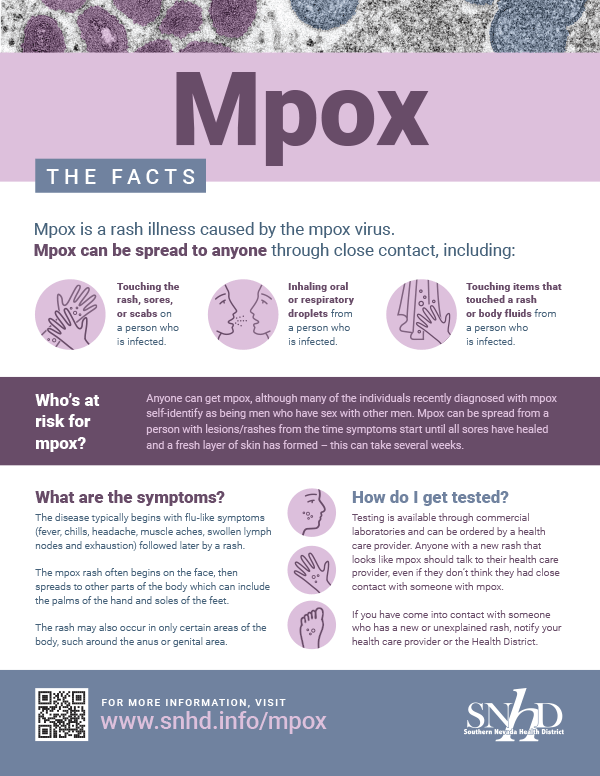
Mpox is contagious and can spread to anyone through close, personal, often skin-to-skin contact including:
- Direct contact with Mpox rash, sores, or scrapes from a person with Mpox. This is believed to be the most common way that Mpox is spreading in the U.S.
- People may contract Mpox after contact with materials that can be contaminated like bed linens, bandages or dishes they have used or surfaces or items they have touched.
- Contact with respiratory secretions.
- This contact can also happen when people are being intimate including:
- Hugging, massage, kissing and prolonged face-to-face contact.
- Oral, anal and vaginal sex or touching the genitals (penis, testicles, labia and vagina) or anus (butthole) of a person with monkeypox.
- Touching fabric and objects during sex that were used by a person with Mpox and that have not been disinfected, such as bedding, towels, fetish gear and sex toys.
Additional ways Mpox can spread include:
- When a person comes into contact with the virus from an infected animal.
- The virus can also cross the placenta from a mother to the fetus.
People who do not have Mpox symptoms cannot spread the virus to others.
Mpox can spread from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. This can take several weeks.
Early symptoms of Mpox are similar to flu. Symptoms of Mpox include:
- Fever
- Headache
- Muscle aches/backache
- Exhaustion
- Swollen lymph nodes
- Chills
- Rash that looks like pimple or fluid filled blisters on the hands, feet, chest, face, genitals, or inside the body including the mouth, vagina or anus.
It takes about seven to 14 days after exposure to develop Mpox, but the timeframe can be five to 21 days.
Mpox typically lasts for two to four weeks.
Mpox and smallpox are from the same virus family called orthopoxvirus. Around the world, smallpox has been eradicated.
A health care provider would order testing to see if you have Mpox. Anyone with a rash that looks like monkeypox should talk to their health care provider, even if they don’t think they had contact with someone who has Mpox.
Mpox is rare and does not spread easily between people without close contact. The threat of Mpox to the general population in the United States is low. Recommendations for those who may have had contact with Mpox virus are available on the CDC’s Exposure Risk Assessment and Public Health Recommendations page.
Mpox and smallpox viruses are similar. Antiviral medications and vaccines developed to protect against smallpox may be used to treat and prevent Mpox infections.
Antivirals may be recommended for people who are more likely to get severely ill, like people who have a weakened immune system.
There are two vaccines currently licensed in the United States to prevent Mpox — JYNNEOS and ACAM200. The Health District is administering the JYNNEOS vaccine to people who meet current eligibility criteria.
The CDC recommends that someone exposed to Mpox should get vaccinated within four days after exposure. This will help prevent the onset of the disease. If someone gets vaccinated between four and 14 days after they are exposed, the vaccine may reduce the symptoms of Mpox but may not prevent the disease.
The CDC does not recommend widespread vaccination against Mpox right now.
While the West African strain is rarely fatal, the symptoms can be very painful and some people might have permanent scars from the rash.
The Centers for Disease Control and Prevention (CDC) has more information on its Mpox webpages. For more information, contact your health care provider or call the Southern Nevada Health District’s Office of Disease Surveillance and Control, (702) 759-1300.
Resources
General
- Signs and Symptoms
- Isolation and Prevention Practices for People with Mpox
- Considerations for Reducing Mpox Transmission in Congregate Living Settings
- What You Need to Know about Mpox if You are a Teen or Young Adult
- Mpox in Animals
- Treatment
- CDC Mpox Website
- 2022 U.S. Mpox Outbreak
- Mpox Frequently Asked Questions
If You Are Sick
Vaccination
- Vaccines
- Interim Clinical Considerations for Use of JYNNEOS and ACAM2000 Vaccines
- How to Administer a JYNNEOS Vaccine Intradermally
- ASPR: JYNNEOS Mpox Vaccine Distribution by Jurisdiction
For Clinicians
- Information For Healthcare Professionals
- Case Definition†
- Clinical Recognition
- Clinician FAQs
- Infection Control: Healthcare Settings
- Infection Control: Home
- Specimen Collection
- Treatment
- Vaccine Guidance
- Duration of Isolation Procedures
- Monitoring Persons Exposed
- Autopsy and Handling of Human Remains
- Clinical Considerations for Treatment and Prophylaxis of Mpox Virus Infection in People with HIV
- Clinical Considerations for Mpox in People Who are Pregnant or Breastfeeding
- Obtaining and Using TPOXX (Tecovirimat)
- Information for Healthcare Professionals
- Information for Veterinarians
- Information for Infection Control at Home
- Monitoring and Risk Assessment for Persons Exposed in the Community
- For Public Health Veterinarians and Animal Health Officials
- Interim Clinical Guidance for the Treatment of Mpox
- Clinician FAQs
- Infection Control: Healthcare Settings
Laboratory
- How to Report Test Results
- Information for Laboratory Personnel
- Preparation and Collection of Specimens
Community
- Pets in the Home
- Safer Sex, Social Gatherings and Mpox
- Prevention
- Preventing Mpox in Congregate Settings
- Reducing Stigma in Mpox Communication and Community Engagement
- Mpox Facts for People Who are Sexually Active
- Travelers’ Health Alert
- Mpox Toolkit for Event Organizers
MMWR
- October 14, 2022 — Mpox Virus Guidance: Infection Control and Prevention in Health Care Settings
- June 29, 2022 — Infection Prevention and Control of Mpox in Health Care Settings
- June 15, 2022 — Updated Case-finding Guidance: Mpox Outbreak- United States, 2022
Mpox Vaccine Eligibility Criteria
- Gay, bisexual, and other men who have sex with men, transgender or nonbinary people who in the past 6 months have had one of the following:
- A new diagnosis of ≥1 sexually transmitted disease
- More than one sex partner
- Sex at a commercial sex venue
- Sex in association with a large public event in a geographic area where mpox transmission is occurring
- Sexual partners of persons with the risks described above
- Persons who anticipate experiencing any of the above
- Persons who had close physical contact with someone known or suspected of having mpox in the last 14 days (could include a sexual partner or someone in the household)
- Persons who have been informed by the Health District that they are a close contact of someone with mpox.
Those who have received their first dose of the vaccine are eligible for the second dose, even if they do not meet any of the current criteria.
Individuals who had Mpox are not eligible for the vaccine. Vaccine clients will be assessed prior to receiving the vaccine to ensure they meet the eligibility requirements.